Subscribe to Stay Informed
LYMES DISEASE
Posted 11/07/25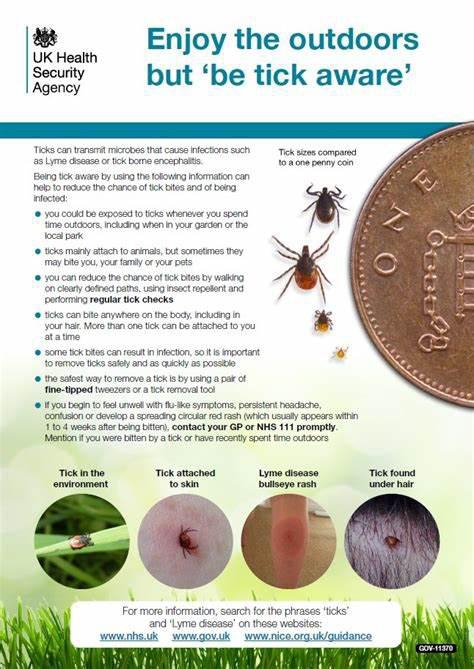
What is Lyme's Disease
Lymes disease is a bacteria causing human infecton caused by the bite of an infected tick, primarily the black-legged tick. It is caused by Borrelia bacteria, which can lead to symptoms such as a bull's-eye rash, joint pain, and fatigue. It left untreated, Lyme disease can affect the skin, joints, heart, and nervious system.
How It Spreads
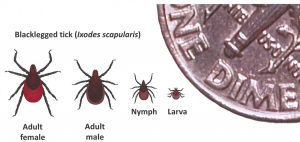
The bacteria that cause Lyme disease in the United States, Borrelia burgdorferi and, rarely, B mayonii, are spread to people through bites of infected ticks. The blacklegged tick (or dear tick, Lxodes scapularis) transmits infection in the northeastern, mid-Atlantic, and north-central United States. Lyme disease can be prevented by avoid tick bites and promptly removing ticks.
The percentage of ticks that are infected ranges from none to over 50%, depending on the area and life stage. Black legged ticks found in most areas of the southeastern United States are almost never infected.
Blacklegged ticks have a 2 to 3 year life cycle. During this time, they go through four life stages: egg, larva, nymph, and adult. After the egg hatches, the larva and nymph each must take a blood meal to develop to the next life stage, and the female needs blood to produce eggs.
Larval and nymphal ticks can become infected with Lyme disease bacteria when feeding on an infected wildlife host, usually a rodent.
How to remove a tick
If you find a tick attached to your skin, remove the tick as soon as possible. Do not wait to go to a healthcare provider to remove the tick. Delaying tick removal to get help from a healthcare provider could increase your risk of getting a diease spread through tick bites, know as tickborne diseases.
- Grasp the tick as close to the skin's surface as possible using clean find-tipped tweezers. If fine tipped tweezers are not available, use regular tweezers or your fingers to grasp the tick. Grasp the tick close to the skin's surface to avoid squeezing the tick's body.
- Pull tick away from the skin with steady, even pressure. Don't twist or jerk the tick. This can cause the tick mouthparts to break off and reamin in the skin. If this happens, your body will naturally push the mouthparts out over time as your skin heals. You can also remove the mouthparts with tweezers. If you cannot remove the mouthparts easily with tweezers, leave them alone.
- Dispose of the live tick by taking one of these steps: place it in a sealed container; wrap it tightly in tape; flush it down the toiler; or put it in alcohol. Do not crush the tick with your fingers.
- After removing the tick, thoroughly clean the bite area and your hands with soap and water, rubbing alcohol, or hand sanitizer.
- If you find a tick attached to you, there may be other tickes on your body. Do a careful tick check to look for other ticks and promptly remove them.
Early signs and symptoms (3 to 30 days after tick bite)
- Fever, chills, headache, fatigue, muscle and joint aches, and swollen lymph nodes may occur in the absence of rash.
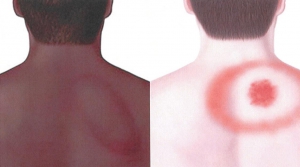 Erythema migrans (EM) rash (see picture)
Erythema migrans (EM) rash (see picture)- Occurs in approximately 70 to 80 percent of infected people
- Begins at the site of a tick bite after a delay of 3 to 30 days (average is about 7 days)
- Expands gradually over several days reaching up to 12 inches (30cm) or more across
- May feel warm to the touch but is rarely itchy or painful
- Sometimes clears as it enlarges, resulting in a target or "bull's-eye" appearance
- May appear on any area of the body.
- Does not always appear as a "classic bull's-eye" rash
Later signs and symptoms (days to months after tick bite)
- Severe headaches and neck stiffness
- Additional EM rashes on other areas of the body
- Facial palsy (loss of muscle tone or droop on one or both sides of the face)
- Arthritis with severe joint pain and swelling, particularly the knees and other large joints.
- Intermittent pain in tendons, muscles, joints, and bones.
- Heart palpitations or an irregular heartbeat
- Episodes of dizziness or shortness of breath
- Inflammation of the brain and spinal cord
- Nerve pain
- Shooting pains, numbness, or tingling in the hands or feet
Testing and Diagnosis
- Healthcare providers consider multiple factors when evaluating a patient for Lyme disease.
- Laboratory diagnosis of Lyme disease relies on a blood test that detects antibodies to the Lyme bacteria. It can take several weeks after infection for the immune system to make enough antibodies to be detected by the test.
- CDC recommends using antibody tests that have been cleared by the U.S. Food and Drug Administration (FDA) and follow a two-step process.
- Some laboratories that do not accept private insurance may be offering tests that are not cleared by the FDA
Diagnosis
When assessing a patient for Lyme disease, your healthcare provider will consider:
- The signs and symptoms of Lyme disease
- The likelihood that you have been exposed to infected blacklegged ticks
- The possibility that other illnesses may cause similar symptoms
- Result of laboratory tests, when indicated.
Laboratory testing
CDC recommends the use of FDA-cleared antibody tests for laboratory diagnosis of Lyme disease. As with antibody tests for other infectious diseases, the accuracy of these tests depends upon how long you've been infected. Antibody tests may appear falsely negative during the first few weeks of infection, typically when a patient has an erythema migrans rash, but FDA-cleared assays have good sensitivity after 4-6 weeks have passed. Once you blood tests positive for antibodies, it will likely continue to do so for months to years, even when the bacteria are no longer present.
Be aware that laboratories that do not accept private insurance may be offering tests that are not cleared or approved by the FDA.
What a diagnosis means
Patients treated with antibiotics in the early stages of the infection usually recover rapidle and completely. Most patients who are treated in later stages of the disease also respond well to antibiotics, although some may have suffered long-term damage to the nervious system or joints.
Because the immune system continues to make the antibodies for months or years after an infection is gone, your blood test will remain positive after the bacteria are no longer present. Unfortunately, these antibodies don't reliably prevent re-infection should you be bitten by another infected tick.
If you need a doctor
In areas where Lyme disease is common, most family practice physicians. general practitioners, and pediatricians are familiar with diagnosing and treating Lyme disease.
Information courtesy of The CDC